Diagnostic test kit Inflaeyez® 100

Diagnostic test kit Inflaeyez® 10
100 diagnostic strips Inflaeyez®
According to the World Health Organization (WHO) and European Centre for Disease Prevention and Control (ECDC), the reason behind the growing antibiotic resistance is excessive and inappropriate use of antibiotics. 1
Antibiotic resistance in ophthalmology involves bacteria that appear on the surface of the eye. Resistant strains of Staphylococcus epidermidis are the most common cause of drug-resistant endophthalmitis. 2
- however, antibiotics are used to treat ca. 60% of all cases of conjunctivitis 5,6
- excessive use of antibiotics results from the difficult differentiation between viral and bacterial conjunctivitis. There are no specific clinical symptoms which could unequivocally indicate a viral or bacterial aetiology behind a case of conjunctivitis. 7
References
- Mazinska B, Hryniewicz W. Antybiotykooporność: przyczyny i konsekwencje. Postępy Mikrobiologii – Advancements of Microbiology 2020, 59, 3, 249–257 doi: 10.21307/PM-2020.59.3.18.
- Asbell PA, Sanfilippo CM, Sahm DF et al. Trends in Antibiotic Resistance Among Ocular Microorganisms in the United States From 2009 to 2018. JAMAOphthalmol. 2020 May 1;138(5):439-450. doi: 10.1001/jamaophthalmol.2020.0155. PMID: 32271355; PMCID: PMC7146550.
- Fariña N, Samudio M, Carpinelli L et al. Methicillin resistance and biofilm production of Staphylococcus epidermidis isolates from infectious and normal flora conjunctiva. Int Ophthalmol. 2017 Aug;37(4):819-825. doi: 10.1007/s10792-016-0339-8. Epub 2016 Sep 10. PMID: 27614460.
- Adebayo A, Parikh JG, McCormick SA et al. Shifting trends in in vitro antibiotic susceptibilities for common bacterial conjunctival isolates in the last decade at the New York Eye and Ear Infirmary. Graefes Arch Clin Exp Ophthalmol. 2011 Jan;249(1):111-9. doi: 10.1007/s00417-010-1426-6.
- Bro T. Rekommendationer följs inte vid okomplicerad konjunktivit - Tillståndet behandlas ofta med topikala antibiotika i strid mot aktuell kunskap (Right treatment of red eyes - prescription of topical antibiotics for infectious conjunctivitis is still common in Sweden). Lakartidningen. 2018 Dec 17;115:FDPX. Swedish. PMID: 30561753.
- Shekhawat NS, Shtein RM, Blachley TS et al. Antibiotic Prescription Fills for Acute Conjunctivitis among Enrollees in a Large United States Managed Care Network. Ophthalmology. 2017 Aug;124(8):1099-1107. doi: 10.1016/j.ophtha.2017.04.034. Epub 2017 Jun 16. PMID: 28624168.
- Rietveld RP, van Weert HC, ter Riet G et al. Diagnostic impact of signs and symptoms in acute infectious conjunctivitis: systematic literature search. BMJ. 2003 Oct 4;327(7418):789. doi: 10.1136/bmj.327.7418.789. PMID: 14525879; PMCID: PMC214099.
INFLAEYEZ® diagnostic assay helps identify the bacterial aetiology of inflammation quickly, and enables the administration of appropriate treatment.
Positive result
topical antibiotic or antibiotic with steroid.
Negative result
antiseptic drops and/ or lubricating drops, and further diagnostics on a needs basis.
How it works
INFLAEYEZ® diagnostic assay enables the administration of appropriate treatment, and reduces the risk of growing resistance to antibiotics used in ophthalmology.
The assay detects the presence of neutrophils in the conjunctival sac discharge.

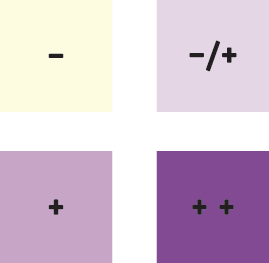
No change (−) or only a slight change of colour (−/+) in the reaction field helps exclude the bacterial aetiology of ocular surface inflammation, and is an indication to apply antiseptic or lubricating eye drops.
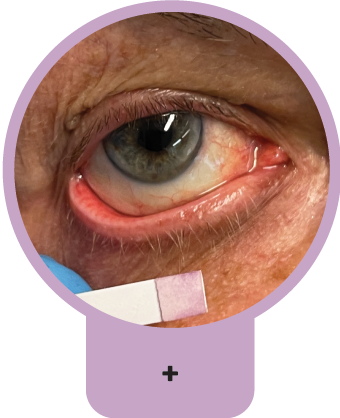
A purple colour (+) of the reaction field indicates the presence of inflammation caused by bacteria, and is a recommendation to use antibiotics or antibiotics combined with steroids.
Results of studies involving the use of INFLAEYEZ® diagnostic assay were presented in 2021 at the following scientific meetings:
M. Oseka, P. Maciejewicz
Leucocyte esterase activity in the conjunctival sac as a marker of the bacterial ocular surface inflammation.
The Association for Research in Vision and Ophthalmology (ARVO) June 2021.
M. Osęka, P. Maciejewicz
The use of a rapid assay for the measurement of leukocyte esterase activity in the detection of acute, bacterial ocular surface inflammation.
52 Congress of the Polish Society of Ophthalmology (Polskie Towarzystwo Okulistyczne - PTO) June 2021.
M. Oseka, P. Maciejewicz
A rapid assay of granulocytic esterase in the discharge of conjunctival sac as a tool for the recognition of bacterial ocular surface inflammation.
European Association for Vision and Eye Research (EVER) October 2021.
Instructions for Use
INFLAEYEZ® diagnostic assay consists of two main elements:
 Diagnostic strip with reaction window
Diagnostic strip with reaction window
 Sterile disposable swab for the collection of specimen from conjunctival sac
Sterile disposable swab for the collection of specimen from conjunctival sac
Simple test procedure
- Remove the diagnostic strip from the pack, and place it on a flat surface, with the diagnostic window facing upward.
- Remove the sterile swab from the pack.
- Collect the specimen from the conjunctival sac with the tip of the swab
- Place the collected material on the diagnostic window
- After ca. 30-60 seconds, compare the change in colour visible in the diagnostic window of the test strip with the result interpretation guide, which is to be found on the packaging.
If there is only a small amount of discharge collected, one should evaluate the change in colour that occurs where the tip of the swab has touched the diagnostic window.
Once the material has been placed on the test strip, one can also wet the diagnostic window with a drop of water for injections. The result obtained in such a manner will be underestimated due to the dilution of the enzyme detected in the collected specimen.
Available INFLAEYEZ® assay packs:
- 100 diagnostic strips + 100 sterile disposable swabs
- 100 diagnostic strips
- 10 diagnostic strips + 10 sterile disposable swabs
Instructions
for use
Instructions
for use
Cases
Clinical cases involving the use of INFLAEYEZ® diagnostic assay, and result interpretation.
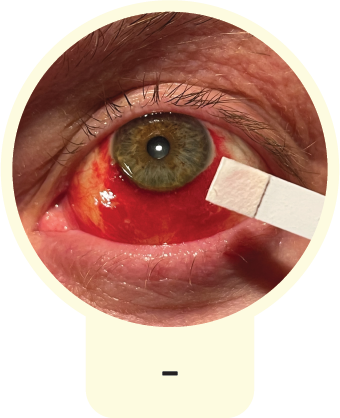
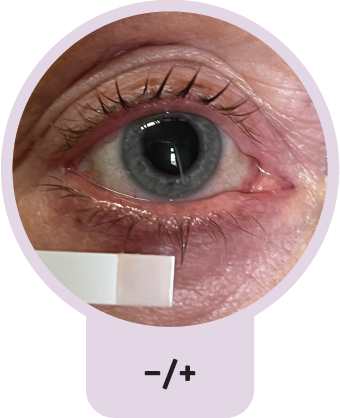
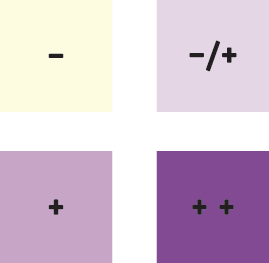
No change (−) or only a slight change of colour (−/+) in the reaction field helps exclude the bacterial aetiology of ocular surface inflammation, and is an indication to apply antiseptic or lubricating eye drops.
A purple colour (+) of the reaction field indicates the presence of inflammation caused by bacteria, and is a recommendation to use antibiotics or antibiotics combined with steroids.